Risk Accumulation
Most infections of mammals are short-term risks. Usually the mammal dies and any adaptive mutations the virus may have gained disappear with the host. But sometimes those variants better adapted to mammals could find their way back into the bird population and replicate for a long time, for example due to scavenging birds. This would increase the pandemic risk for a long time. It could also increase the ability of birds to infect mammals.
In a very simplified model, 4 mutations are needed for aerosol-based mammal-to-mammal transmission as shown in the Fouchier et al gain-of-function experiment. One of those mutations circulating in the bird population would reduce the number of mutations to be gained in a mammal (population) from 4 to 3. Of course reality is much more complex, but some adaptations clearly increase the pandemic risk.
However the prevalence of mutations in the various variants of H5N1 is quite diverse. While the PB2-E627K prevalence in clade 2.2 is 92.1%, it is only 1.1% in clade 2.3 and 1.0% in clade 2.3.4.4b, which has caused the current panzootic. So far this seems like a positive development. But the spread of the virus and the absolute number of cases have increased. Some concerning mutations associated with mammals don't seem to be decrease the transmissibility in bird populations. Others are only a minor evolutionary disadvantage and may become more prevalent at any time.
And there are signs of these adaptations circulating in wild birds.
The most worrying H5N1 variant detected so far, although not yet peer-reviewed, was found in a bird with a preference for scavenging, the Red Tailed Hawk. This variant is capable of ferret-to-ferret transmission by direct contact.
A PB2-T271A mutation has been found in all infected animals from the mixed farm in Brescia, Italy. This includes five dogs, one cat, and poultry. This implies that the wild bird vector already carried the mutation.
Another concerning development is that the virus managed to infect approximately 30 fur farms in Finland in a short amount of time. Before there has been only a single infected fur farm in Galicia, Spain in 2022. This may indicate an improved ability to infect mammals and widespread circulation within the bird population, with the potential to spread to many more fur farms.
Just as in Spain there is a high probability of mammal-to-mammal transmission on the fur farms in Finland, which makes this very concerning.
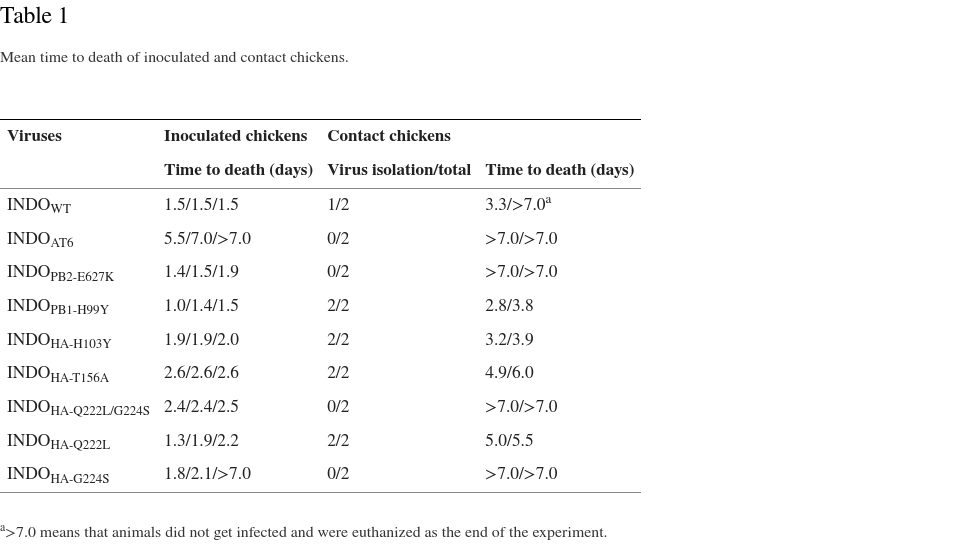
PB2-E627K and HA-T156A or functionally similar mutations are found fairly often in H5N1 viruses. Variants with the mutations PB1-H99Y, HA-H103Y, and HA-Q222L have been found to be transmissible between birds in laboratory experiments. Variants with HA-G224S were not transmissible between birds. All mutations combined reduced the virulence significantly, an evolutionary disadvantage. While in reality adaptations specifically to the human immune system have to be considered, the basic idea that most mutations required for mammal-to-mammal transmission could at least locally accumulate in avian hosts seems to be realistic.
A very concerning recent discovery is the HA-N193D mutation, which enables dual receptor binding specificity and other dangerous properties with just a single mutation.
The confirmed spillback of the reassorted virus from infected cows into multiple poultry farms, cats, a racoon, and at least three wild birds (14 as of June 2024) elevates the risk.
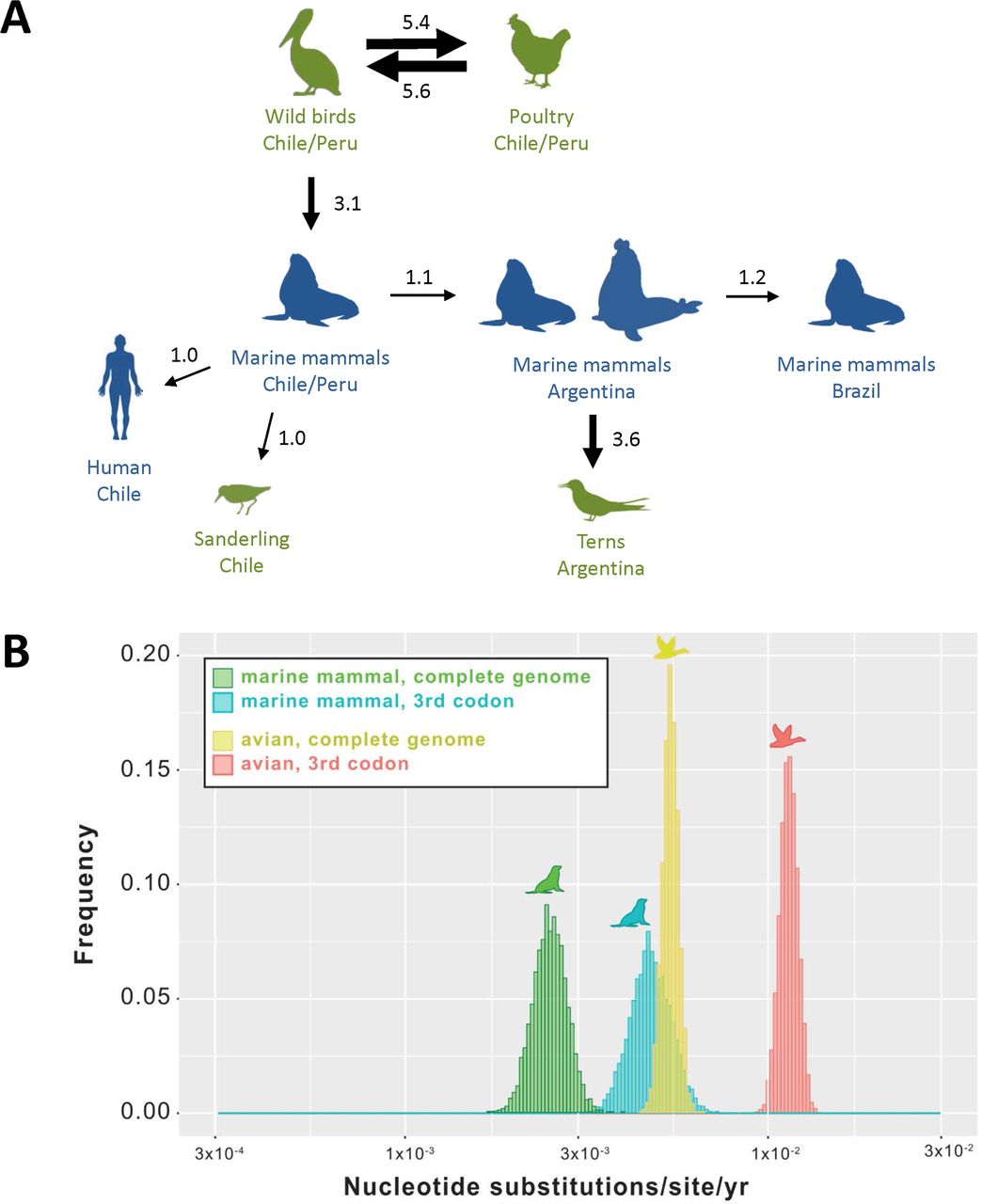
There was possible evidence of mammal-to-mammal transmission or an avian reservoir in South America in form of a cluster of rare PB2-D701N mutations including a bird, two sea lions, and a human. However the initial phylogenetic analysis showed that these rare mutations probably developed independently from each other. In another case in Argentina however, the sea lions carried the same rare mutations as a tern from the same area, PB2-Q591K and PB2-D701N, suggesting circulation in local birds and transmission of mammalian adaptations from mammals to bird. A recent pre-print provides evidence phylogenetic evidence for mammal-to-mammal transmission among elephant seals in South America. Furthermore the pre-print now provides evidence for spillback into terns and a for distinct clade present in terns and elephant seals across South America, including the human case. The repeated spillbacks into birds could result in several adaptations to mammals circulating in the bird population.
H3N8
With H3N8 another avian influenza virus is proving that acquisition of most of the mutations discussed above is possible, although the specimen in question is from a human infection.
H5N1 Spread
Another concerning development is the continuous spread of H5N1. It seems likely that H5N1 will sooner or later arrive on the remaining uninfected continent, Australia. This would maximize the number of available hosts, with H5N1 circulating almost everywhere. With hardly any geographical boundaries and a broad host range, H5N1 will probably be a persistent threat for decades. And it may continue to adapt to mammals. The unprecedented H5N1 infections of cows seemingly related to milking demonstrate how a large number of infected birds can lead to unexpected widespread infections, leading to spillovers into other species from the cows, including wild birds, cats and a racoon, and even back into poultry and from there into humans. A reassortment between clade 2.3.2.1c and clade 2.3.4.4b found in a human illustrates how the large number of circulating viruses may result in dangerous new variants.